Online identity vetting for state benefits
Health care ushers in secure access for citizen e-services
02 September, 2014
category: Corporate, Digital ID, Government, Health, Library
Anyone who has applied for social service benefits knows that reporting to a brick-and-mortar office can be painful at the best of times. It is for this reason that many states are turning to online identity vetting and application processing.
But while the jump to online benefits applications makes sense for many reasons, not the least of which is convenience, there are vital concerns that must to be addressed to ensure these systems are secure as well as easy to use.
Vetting an identity online can be a tricky business, but thankfully, there are entities working to ensure that a citizen applying for Medicaid, child welfare or similar service is who they claim to be.
Big data processing
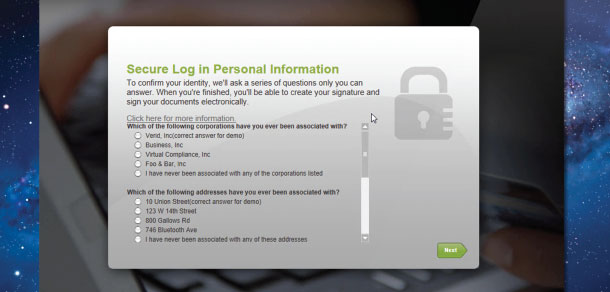
How do you establish a person’s identity via an online portal? LexisNexis is one of a handful of companies using public data to offer state agencies a level of assurance that a person is who they claim to be.
“We have identity records for 585 million people alive or deceased and can provide that data to commercial and government organizations to actively identify their user bases,” explains Alisoun Moore, senior director of government health care at LexisNexis Risk Solutions.
Companies like LexisNexis can provide access to the history of identity information. “If you register to vote, buy a car or apply for a driver license – things you typically do between the ages of 16 to 21 – we start tracking you from that moment forward,” says Moore. “It’s all public records information.”
“We take information from about 10,000 sources of public record data, all standardized under Fair Credit Reporting Act,” she explains.
Public records contain virtually all the information that a state agency needs to verify a citizen’s identity. “If you rent an apartment or purchase a home, that address is public record and can be used to establish residency,” explains Moore. “If you find that a person has several addresses that are current, for example, that may tip off that the person may have some type of residency issue or discrepancy.”
This public information can then be built into the front end of an application for identity proofing. “The state of Florida has implemented an identity vetting process before the citizen even applies for care,” Moore explains. “Vetting in this instance is done via a short quiz using questions like ‘Did you live at this address in 2001?’”
As Moore explains, Florida has seen a noticeable drop in cases of benefits application fraud following the additional vetting measures, as fraudulent users – who more than likely don’t know the answers to those questions – simply go away.
The same vetting process can be used when you apply for a driver license. “The DMV checks your driving record, which is public information,” says Moore. “Then the LexisNexis database immediately provides information that allows the DMV to properly identify the individual who claims a specific identity.”
This stands in stark contrast to how state-level identity vetting has traditionally been conducted. “In-person vetting relies on a credential – driver license, passport, birth certificate, etc. – to determine that you are who you say you are,” explains Moore. “An agency employee checks to make sure that signatures match. That is how identity vetting has taken place for decades and continues today in many instances.”
The proverbial monkey wrench, however, emerged with the electronic era. “It’s more efficient for government agencies to serve citizens via online applications, but that adds a big twist to identity vetting,” Moore says.
The emergence of the Affordable Care Act – otherwise known as Obamacare – has greatly expedited the jump to online benefits applications.
“The Affordable Care Act did something incredible, in that it incentivized health care in the U.S. – a $2.5 billion industry – to go digital,” says Moore. “It also incentivized health care providers to actually implement electronic health records, and it invested tens of millions of dollars to build and digitally operate health insurance exchanges.”
Identifying people electronically now becomes key to this new digital health care world, and as Moore explains, it’s just the beginning. “This just started. Imagine things in another five years,” says Moore. “Wouldn’t it be nice if your health information could be securely and efficiently shared?”
For now, the online portal is ground zero for digital benefits applications, with the longer-term future likely to leverage predictive analytics to better safeguard applicants.
“What we see for the future is the evolution of identity analytics,” she says. “For instance, you would be able to predict what type of fraudulent activity may occur with a particular application or service, as well what things fraudsters might try.”
The key to knowledge based authentication technology is that it attempts to nip fraud in the bud. Typically fraud is identified through a tip on a hotline and an enforcement entity investigates and then prosecutes the fraud. Moore believes there is a better way. “Verify and authenticate the identity of an individual up front, and you can ensure that the fraud never occurs in the first place,” she says.